|
Iodine is a trace mineral that is vital to the function of the thyroid gland. The human body does not make iodine, so all iodine intake must come from either our diet or from supplements.
Magnesium has an effect on more than 300 bodily chemical reactions. This includes maintaining heart health, sustaining blood vessels, boosting and maintaining energy levels, producing new cells and proteins, and enabling enzyme activity.
|
|
Imaging Services >
Breast - MRI
Magnetic Resonance Imaging (MRI) - Breast
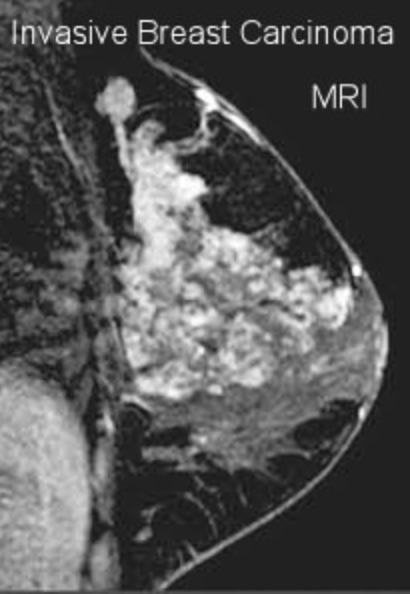
Magnetic resonance imaging (MRI) of the breast uses a powerful magnetic field, radio waves and a computer to produce detailed pictures of the structures within the breast. It is primarily used as a supplemental tool to breast screening with mammography or ultrasound. It may be used to screen women at high risk for breast cancer, evaluate the extent of cancer following diagnosis, or further evaluate abnormalities seen on mammography. Breast MRI does not use ionizing radiation, and it is the best method for determining whether silicone breast implants have ruptured. Tell your doctor about any health problems, recent surgeries or allergies and whether there's a possibility you are pregnant. The magnetic field is not harmful, but it may cause some medical devices to malfunction. Most orthopedic implants pose no risk, but you should always tell the technologist if you have any devices or metal in your body. Guidelines about eating and drinking before your exam vary between facilities. Unless you are told otherwise, take your regular medications as usual. Leave jewelry at home and wear loose, comfortable clothing. You may be asked to wear a gown. If you have claustrophobia or anxiety, you may want to ask your doctor for a mild sedative prior to the exam.
What is MRI of the Breast?Magnetic resonance imaging (MRI) is a noninvasive medical test that physicians use to diagnose medical conditions. MRI uses a powerful magnetic field, radio frequency pulses and a computer to produce detailed pictures of organs, soft tissues, bone and virtually all other internal body structures. MRI does not use ionizing radiation (x-rays). Detailed MR images allow physicians to evaluate various parts of the body and determine the presence of certain diseases. The images can then be examined on a computer monitor, transmitted electronically, printed or copied to a CD or uploaded to a digital cloud server. MRI of the breast offers valuable information about many breast conditions that cannot be obtained by other imaging modalities, such as mammography or ultrasound. What are some common uses of the procedure?MRI of the breast is not a replacement for mammography or ultrasound imaging but rather a supplemental tool that has many important uses, including:
How should I prepare?You may be asked to wear a gown during the exam or you may be allowed to wear your own clothing if it is loose-fitting and has no metal fasteners. Guidelines about eating and drinking before an MRI exam vary with the specific exam and with the imaging facility. Unless you are told otherwise, you may follow your regular daily routine and take food and medications as usual. Some MRI examinations may require you to receive an injection of contrast material into the bloodstream. The radiologist, technologist or a nurse may ask if you have allergies of any kind, such as an allergy to iodine or x-ray contrast material, drugs, food, or the environment, or if you have asthma. The contrast material most commonly used for an MRI exam contains a metal called gadolinium. Gadolinium can be used in patients with iodine contrast allergy. It is far less common for a patient to have an allergy to a gadolinium-based contrast agent used for MRI than the iodine-containing contrast for CT. However, even if it is known that the patient has an allergy to the gadolinium contrast, it may still be possible to use it after appropriate pre-medication. Patient consent will be requested in this instance. You should also let the radiologist know if you have any serious health problems, or if you have had any recent surgeries. Some conditions, such as severe kidney disease, may prevent you from being given gadolinium contrast for an MRI. If you have a history of kidney disease or liver transplant, it will be necessary to perform a blood test to determine whether the kidneys are functioning adequately. Women should always inform their physician or technologist if there is any possibility that they are pregnant. MRI has been used for scanning patients since the 1980s with no reports of any ill effects on pregnant women or their unborn babies. However, because the unborn baby will be in a strong magnetic field, pregnant women should not have this exam in the first three to four months of pregnancy unless the potential benefit from the MRI exam is assumed to outweigh the potential risks. Pregnant women should not receive injections of gadolinium contrast material except when absolutely necessary for medical treatment. If you have claustrophobia (fear of enclosed spaces) or anxiety, you may want to ask your physician for a prescription for a mild sedative prior to your scheduled examination. Jewelry and other accessories should be left at home, if possible, or removed prior to the MRI scan. Because they can interfere with the magnetic field of the MRI unit, metal and electronic items are not allowed in the exam room. In addition to affecting the MRI images, these objects can become projectiles within the MRI scanner room and may cause you and/or others nearby harm. These items include:
In most cases, an MRI exam is safe for patients with metal implants, except for a few types. People with the following implants cannot be scanned and should not enter the MRI scanning area:
You should tell the technologist if you have medical or electronic devices in your body. These objects may interfere with the exam or potentially pose a risk, depending on their nature and the strength of the MRI magnet. Many implanted devices will have a pamphlet explaining the MRI risks for that particular device. If you have the pamphlet, it is useful to bring that to the attention of the scheduler before the exam and bring it to your exam in case the radiologist or technologist has any questions. Some implanted devices require a short period of time after placement (usually six weeks) before being safe for MRI examinations. Examples include but are not limited to:
If there is any question of their presence, an x-ray may be taken to detect and identify any metal objects. In general, metal objects used in orthopedic surgery pose no risk during MRI. However, a recently placed artificial joint may require the use of another imaging procedure. Patients who might have metal objects in certain parts of their bodies may also require an x-ray prior to an MRI. You should notify the technologist or radiologist of any shrapnel, bullets, or other pieces of metal that may be present in your body due to prior accidents. Foreign bodies near and especially lodged in the eyes are particularly important because they may move during the scan, possibly causing blindness. Dyes used in tattoos may contain iron and could heat up during an MRI scan, but this is rare. Tooth fillings and braces usually are not affected by the magnetic field, but they may distort images of the facial area or brain, so you should let the radiologist know about them. What does the equipment look like?
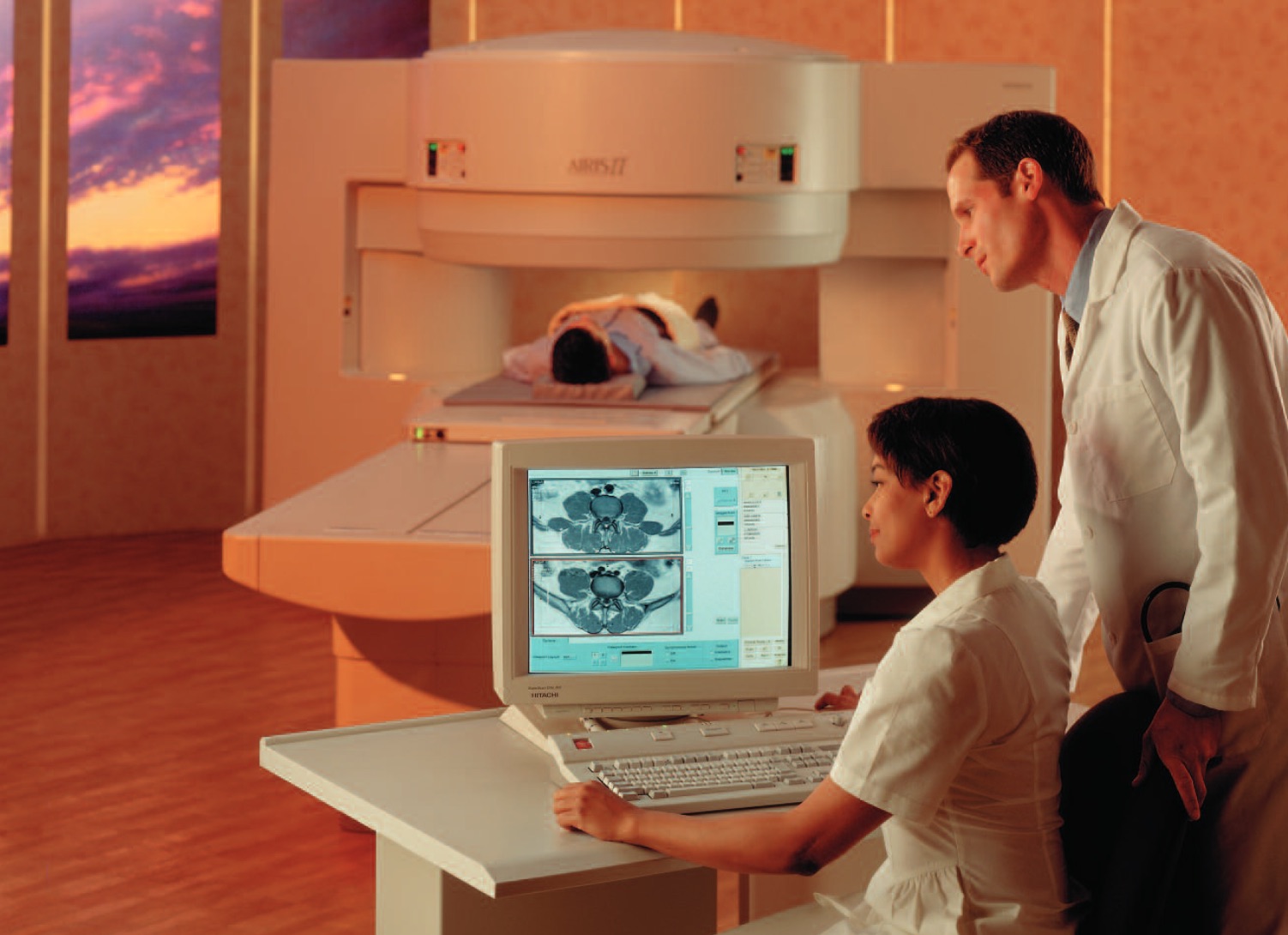
The traditional MRI unit is a large cylinder-shaped tube surrounded by a circular magnet. You will lie on a moveable examination table that slides into the center of the magnet. Some MRI units, called short-bore systems, are designed so that the magnet does not completely surround you. Some newer MRI machines have a larger diameter bore which can be more comfortable for larger size patients or patients with claustrophobia. Other MRI machines are open on the sides (open MRI). Open units are especially helpful for examining larger patients or those with claustrophobia. Newer open MRI units provide very high quality images for many types of exams. Older open MRI units may not provide this same image quality. Certain types of exams cannot be performed using open MRI. For more information, consult your radiologist. The computer workstation that processes the imaging information is located in a separate room from the scanner. How does the procedure work?Unlike conventional x-ray examinations and computed tomography (CT) scans, MRI does not utilize ionizing radiation. Instead, radiofrequency pulses re-align hydrogen atoms that naturally exist within the body. This does not cause any chemical changes in the tissues. As the hydrogen atoms return to their usual alignment, they emit different amounts of energy depending on the type of body tissue they are in. The MR scanner captures this energy and creates a picture of the tissues scanned based on this information. The magnetic field is produced by passing an electric current through wire coils in most MRI units. Other coils, located in the machine and in some cases, placed around the part of the body being imaged, send and receive radio waves, producing signals that are detected by the coils. The electric current does not come in contact with the patient. A computer then processes the signals and generates a series of images, each of which shows a thin slice of the body. The images can then be studied from different angles by the interpreting radiologist. Frequently, the differentiation of abnormal (diseased) tissue from normal tissues is better with MRI than with other imaging modalities such as x-ray, CT and ultrasound. How is the procedure performed?MRI examinations may be performed on outpatients or inpatients. You will be positioned on the moveable examination table. Straps and bolsters may be used to help you stay still and maintain the correct position during imaging. For an MRI of the breast, you will lie face down on a platform specially designed for the procedure. The platform has openings to accommodate your breasts and allow them to be imaged without compression. The electronics needed to capture the MRI image are actually built into the platform. It is important to remain very still throughout the exam. This is best accomplished by making sure you are comfortable and can relax rather than trying to actively hold still tensing your muscles. Be sure to let the technologist know if something is uncomfortable, since discomfort increases the chance that you will feel the need to move during the exam. If MRI of the breast is being performed for the sole purpose of determining if you have a ruptured breast implant, you will not be given contrast material. If the exam is being performed for any other reason, you will need to have a contrast material injected intravenously. MRI of the breast without contrast material is inadequate for identifying breast cancers. If a contrast material will be used in the MRI exam, a physician, nurse or technologist will insert an intravenous (IV) catheter, also known as an IV line, into a vein in your hand or arm. A saline solution may be used to inject the contrast material. The solution will drip through the IV to prevent blockage of the IV catheter until the contrast material is injected. You will be placed into the magnet of the MRI unit and the radiologist and technologist will perform the examination while working at a computer outside of the room. If a contrast material is used during the examination, it will be injected into the intravenous line (IV) after an initial series of scans. Additional series of images will be taken during or following the injection. When the examination is complete, you may be asked to wait until the technologist or radiologist checks the images in case additional images are needed. Your intravenous line will be removed. MRI exams generally include multiple runs (sequences), some of which may last several minutes. The imaging session lasts between 30 minutes and one hour and the total examination is usually completed within an hour and a half. MR spectroscopy, which provides additional information on the chemicals present in the body's cells, may also be performed during the MRI exam and may add approximately 15 minutes to the total exam time. What will I experience during and after the procedure?Most MRI exams are painless. However, some patients find it uncomfortable to remain still during MR imaging. Others experience a sense of being closed-in (claustrophobia) while in the MRI scanner. Therefore, sedation can be arranged for those patients who anticipate anxiety, but fewer than one in 20 require medication. It is normal for the area of your body being imaged to feel slightly warm, but if it bothers you, notify the radiologist or technologist. It is important that you remain perfectly still while the images are being recorded, which is typically only a few seconds to a few minutes at a time. For some types of exams, you may be asked to hold your breath. You will know when images are being recorded because you will hear tapping or thumping sounds when the coils that generate the radiofrequency pulses are activated. You will be able to relax between imaging sequences, but will be asked to maintain your position as much as possible. You will usually be alone in the exam room during the MRI procedure. However, the technologist will be able to see, hear and speak with you at all times using a two-way intercom. Many MRI centers allow a friend or parent to stay in the room as long as they are also screened for safety in the magnetic environment. You may be offered or you may request earplugs to reduce the noise of the MRI scanner, which produces loud thumping and humming noises during imaging. MRI scanners are air-conditioned and well-lit. Some scanners have music to help you pass the time. When the contrast material is injected, it is normal to feel coolness and a flushing sensation for a minute or two. The intravenous needle may cause you some discomfort when it is inserted and once it is removed, you may experience some bruising. There is also a very small chance of irritation of your skin at the site of the IV tube insertion. If you have not been sedated, no recovery period is necessary. You may resume your usual activities and normal diet immediately after the exam. A few patients experience side effects from the contrast material, including nausea and local pain. Very rarely, patients are allergic to the contrast material and experience hives, itchy eyes or other reactions. If you experience allergic symptoms, a radiologist or other physician will be available for immediate assistance. Who interprets the results and how do I get them?A radiologist, a physician specifically trained to supervise and interpret radiology examinations, will analyze the images and send a signed report to your primary care or referring physician, who will share the results with you. Follow-up examinations may be necessary. Your doctor will explain the exact reason why another exam is requested. Sometimes a follow-up exam is done because a potential abnormality needs further evaluation with additional views or a special imaging technique. A follow-up examination may also be necessary so that any change in a known abnormality can be monitored over time. Follow-up examinations are sometimes the best way to see if treatment is working or if a finding is stable or changed over time. What are the benefits vs. risks?Benefits
Risks
What are the limitations of MRI of the Breast?High-quality images are assured only if you are able to remain perfectly still and follow breath-holding instructions while the images are being recorded. If you are anxious, confused or in severe pain, you may find it difficult to lie still during imaging. A person who is very large may not fit into the opening of certain types of MRI machines. The presence of an implant or other metallic object sometimes makes it difficult to obtain clear images due to streak artifacts from the metallic objects. Patient movement can have the same effect. A very irregular heartbeat may affect the quality of images obtained using techniques that time the imaging based on the electrical activity of the heart, such as electrocardiography (EKG). Although there is no reason to believe that magnetic resonance imaging harms the fetus, pregnant women usually are advised not to have an MRI exam during the first trimester unless medically necessary. MRI may not always distinguish between cancer tissue and fluid, known as edema. MRI typically costs more and may take more time to perform than other imaging modalities. Sometimes a benign (non-cancerous) piece of tissue in the breast can take up the contrast material and show up as a bright spot on the image. Often, the radiologist can tell by the appearance of the tissue whether it is cancer or not. When it is not possible, other testing such as ultrasound of that specific spot or a biopsy may be needed. If additional testing or biopsy shows no cancer, it is called a false-positive test result. |
|
|

OPEN 24 HOURS: ACCIDENT EMERGENCY, LAB SERVICES, IMAGING SERVICES & PHARMACY